As a hip and knee surgeon at HSS, I am blessed and humbled to be able to help people get better. I know from the inside what a special place this is – in every aspect, from the nurses, to the security guards, to building services – people here bring pride to work, and smile as the pass in the hallways; and this culture manifests itself in consistently excellent outcomes and high patient satisfaction. But I did not expect to develop an understanding from the other side.
“This is the most reproducible operation I do”. With these words Dr. Drakos and I began our journey in July 2021. Numerous sprains as a kid playing basketball left me with a “loose” ankle, but without symptoms if I kept it strong. I reinjured my ankle while training for an upcoming surf trip. I pushed really hard into the ankle while turning away to simulate a turn on a big wave, and felt and heard a crunch deep in the ankle and all the way up the middle of my calf to the knee. So, I limped back home. This was in the midst of the first COVID-19 surge in NYC. Dr. Drakos was leading the efforts of orthopaedic surgeons volunteering to help the medical doctors and anesthesiologists take care of Covid patients at HSS. I was limping around the hospital while rounding on Covid patients with full infection prevention protective gear, and it became clear that this was not going to work, so I went to see the boss.
When he asked me what I felt, I could only say that when I stepped on it if felt “just wrong, horribly wrong”. He responded – yep, instability. We tried conservative treatment for a while, but it wasn’t working. We got a stress x-ray, which was decidedly uncomfortable – and well mimicked the feeling of “wrong” of instability. The separation between the bones with stress was impressive: surgery – a Brostrom and a Tightrope. Such cute names for operations. We proceeded with surgery following week. In the HSS ambulatory surgery center everything went smoothly. Warm greetings, with smiling eyes peeking over masks. My anesthesiologist, Dr. Sang Jo Kim, exuded cool confidence. I felt nothing, and remember nothing, and upon awakening had no pain.
Dr. Drakos was very clear about what to expect after surgery. “Your ankle should be elevated above your heart 24/7, dropping only when absolutely necessary”. Boy, was he right. Once the anesthetic block wore off, anytime the foot came below my heart, it felt like it was on fire and going to explode, but if I kept it up, I felt almost nothing, so I kept it up.
By the end of the second week it was feeling a little better, and I could walk around for a few minutes. So I took my crutches and headed over to the park. When the body is unaccustomed to walking with crutches, the fatigue that it brings is notable. Getting to the park occurred in stages, but arrival was sublime after 2 weeks in a bed.
“Three months to feel normal at work, 6 months to get back to sports”. This was another quote that I hung on as I assessed my progress every day. Once I was allowed into the boot (cam walker) I could return to see patients part-time, and occupy my mind that way. Thinking about others is easier than thinking about yourself. Dr. Drakos guided me to purchase a special peg-leg mobility device, which allowed me to walk non-weight-bearing without using my arms. This was the first real sense of independence that I tasted. Now I could operate again, which he allowed at 4 weeks. The silent burden of walking around with a mobility device was surprising as I only noticed being physically and emotionally fatigued after the walk from the OR to the office between cases, and was “done” and in bed by 9 every night. Rest was not only essential, it was unavoidable. After a month of this, I could put weight on the leg – the next graduation.
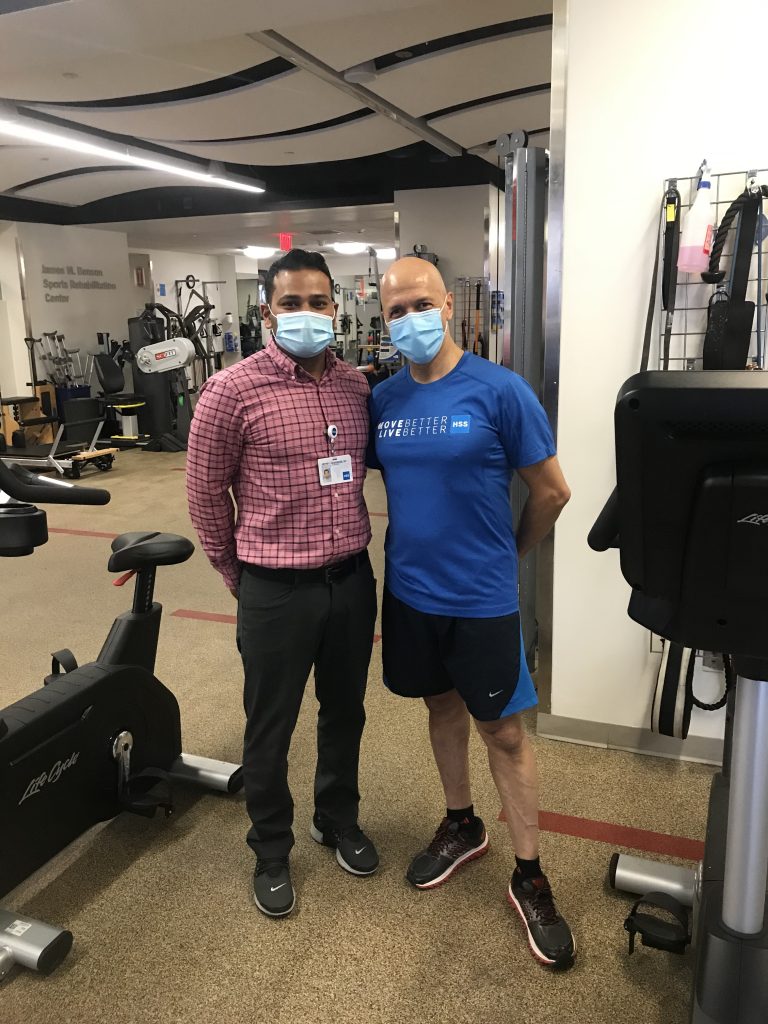
One of the most important aspects of this journey has been the patient-physical therapist relationship. I had 4 awesome therapists, Harrison Herman, Kimberly Baptiste, Amit Gohil, and Jeff Varghese, who guided me through this process. Recovery is not linear. One gets better, and better, and then goes backwards as the limits of ability are tested. The experience, wisdom, and personal qualities of each member of this therapy team was absolutely instrumental in giving me the confidence to go forwards, and the humility to accept the setbacks that are an inherent part of the process. I understood this intellectually as a surgeon. I now understand it emotionally and viscerally as a patient, and deeply appreciate its power to shape the recovery process.
On Christmas Eve, Jeff put me on the treadmill to run for 10 minutes for the first time in 9 months. What a gift! 2 weeks later… a very slow, but delicious 2-mile run. And last week, just under 6 months post op, I returned to surfing. And the words rung in my ear “…the most reproducible operation I do”. My journey continues as the strength and springiness continue to improve almost weekly. I give thanks for great surgery, adept anesthesia, awesome therapy, an amazing OR and office staff, and a wonderful place to work.
Thank you, Dr. Drakos, for keeping your promises. I experience your skill every single day.